
STICK-TO-SKIN: Behind The Science
(re)think medical adhesives…
Medical-grade pressure sensitive adhesives (PSAs) are already widely used in all kind of healthcare applications. Selecting the right adhesive, however, is critical to the success of a new medical device or patch as this can seriously affects its performance as well as its manufacturing method. Thanks to our extensive network of medical-grade PSA suppliers, Tacon/Matrix is able to offer a wide range of tapes for each specific application. Last week, our team attended a technical training with 3M to understand the ‘Science of Skin’ in order we can give our customers additional support (cfr. expertise and knowledge) to select the right medical-grade PSA.
We cannot hide it anymore: medical devices are essential in today’s society! Thanks to Covid-19 pandemic, for example, wearable remote patient monitoring devices came highly to the forefront to reduce pressure on hospital care. The market demands, however, increased wear time of medical devices, but can we make them more convenient by increasing wear time without compromising skin safety? Let’s explain it to you by showing the ‘Science of Skin’.
The human skin is the outer covering of the body and largest organ of the integumentary system. The skin has up to seven layers of ectodermal tissue and guard the underlying muscles, bones, ligaments and internal organs. Due to the skin’s function, many factors affect skin adhesion and wear time of medical-grade PSAs:
- Contaminated surface: top layer of skin needs to be cleaned (e.g. sweat, oil) before creating physical attraction to it.
- Breathing, sensitive surface: vapour/moisture exchange to control body temperature
- Low surface energy: skin is in the same category as Teflon, silicone
- Hairy skin: remove hair before applying any PSA
- Surface bacteria: complete recolonization of surface bacteria can occur within 18 hours of antiseptic application as resident bacteria are also found in biofilms within the hair follicles and sebaceous glands.
- Cell renewal cycle
- Rough texture
- Elastic surface
One of the main epidermal functions is moisture management: about 15% of skin surface is covered with water (flat, dead keratinized cells). Due to this, medical-grade PSAs for long wear-time applications should be breathable. For example: white discoloration of human skin after wearing plasters is caused by unbreathable materials and thus, moisture cannot be drained off. Another important phenomena is aging as it reduces skin functionality. Young persons have a thick dermis layer which gets thinner over the years. The connection between the epidermis – and dermis layer losses strength and for that reason, older people suffer from damage caused by releasing adhesives. Don’t make following mistake: for short wear-time applications, don’t use PSAs with very high adhesion because it can damage (y)our skin!
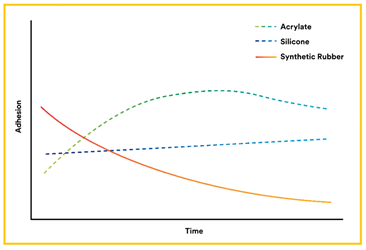
Up to the next question: ‘how well is the adhesive working on the skin’? Skin adhesion is an abstract concept, which cannot be measured by any standard equipment. Due to the complicated skin’s surface, it is absolutely meaningless to compare adhesion to steel (as described in datasheets) with adhesion to skin. There is no proven correlation between both performances. The skin adhesion of different adhesive types, on the other hand, has been extensively investigated:
- Synthetic rubber: barely used as medical-grade PSA, as it traps lot of moisture under adhesive and adhesion decreases over time.
- Acrylate: used a lot as medical-grade PSA, as adhesion is building up over time and acrylate polymers are breathable to enhance moisture exchange. Good peel adhesion and shear resistance.
- Silicone: used a lot as medical-grade PSA, as it has a low peel adhesion but comparable shear to acrylate adhesives. It has almost full attachment after application, breathable in combination with right backing and low trauma on removal due to low peel adhesion.
Nevertheless, medical-grade PSAs can also cause skin injury (MARSI = Medical Adhesive Related Skin Injury). Skin injury results when the skin-to-adhesive attachment is stronger than the skin-to-skin attachment. To avoid this, it is required to select the right type of adhesive. Removing silicone gel adhesive causes far less stresses than acrylate adhesive, because the gel adhesive flexes and brakes the bond in its elastic part of the adhesive layer. In addition, top layer of skin cells are less removed by using silicone adhesives instead of acrylic adhesives due to the peel behaviour.
Some examples of skin injuries are:
- Skin stripping
- Skin tear
- Tension injury
- Maceration
- Allergic contact dermatitis
- Irritant contact dermatitis
- Folliculitis

The selection of the right medical-grade PSAs depends on a lot of significant factors, but following 4 main criteria are key:
- What is the application?
- Where will it be worn?
- How long will it be worn?
- Who will wear it?
If you have additional request for your stick-to-skin application, our R&D – and sales team is always available to assist in answering those questions and identifying solutions. We will definitely recommend to perform a wear-time study and for that, we can provide you with the right information and sample material!
Tacon/Matrix, your partner solving adhesive converting challenges!
Do you want to share your idea? Please contact us through below form.




